Today's Diets: Do They Work? Fact versus Fiction
ABSTRACT: Most of our patients have tried at least one diet in their lifetime. As physicians, we must understand the various dieting fads to best offer advice that encourages long-term lifestyle changes through healthy, nutritious eating. This article breaks down today’s popular diets to give physicians the tools they need to address patient inquiries.
Primary care physicians are regularly tasked with managing the biggest healthcare challenges today. As obesity, type 2 diabetes, and cardiovascular disease become more common, physicians must hone their abilities to treat patients with these disorders.
Lifestyle modification—including dietary counseling—is a cornerstone of treatment; thus, it follows that primary care physicians should be experts on providing nutritional recommendations to patients. However, surveys of practicing physicians reveal that fewer than half provide specific guidance on diet, physical activity, or weight control.1 Too often, physicians simply tell patients they need to “lose weight” without offering specific strategies to help them actually do so. Surveys of resident physicians show that despite recognizing nutritional counseling as a priority, most lack the knowledge and confidence to provide this service to patients.2 As mainstream knowledge of nutrition is constantly molded by dubious marketing claims and new fad diets, physicians are further challenged to use evidence-based medicine.
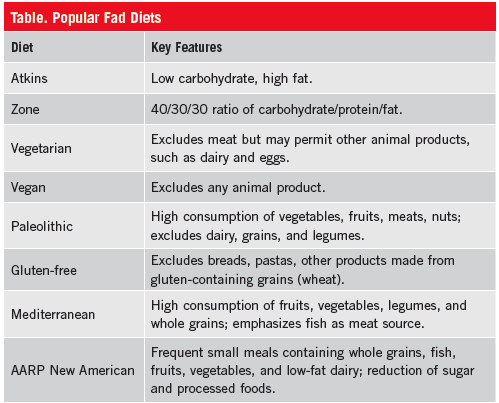
Patients often have diet questions for their physicians and expect their doctor to be a credible source of nutritional information.3 To help primary care physicians more adequately address patient concerns, this article reviews common diets that have achieved mainstream popularity (Table) and helps separate fact from fiction when it comes to health benefits.
THE LOW-CARBOHYDRATE DIETS
Low-carbohydrate diets are based on the theory that limited carbohydrate intake will force the body to use stored fat as fuel through ketosis, resulting in fat loss.
Since the widespread popularity of the Atkins diet in the late 1990s, low-carbohydrate diets have taken on various forms. The Atkins plan is the most well known and consists of a four-phase plan that, in addition to a drastic reduction in and subsequent stepwise reintroduction of carbohydrate, promotes high fat intake.4 The Zone plan aims to rein in elevated insulin levels by following a 40/30/30 ratio of carbohydrates/protein/fat.4 The South Beach plan consists of three phases based on eating specific types of carbohydrates and fats.4 Dieters are generally advised to avoid breads, pastas, rice, and other carbohydrates, though complex carbohydrates may be permitted in limited amounts.
Dieters who followed the Atkins or Zone diet for 12 months experienced modest yet statistically significant weight reductions compared to baseline.5 However, the greatest weight change from baseline for both diets was noted after 2 months, suggesting that both of these diets can induce a rapid weight loss that levels off and even increases slightly by 12 months. Approximately 25% of subjects were able to sustain a clinically significant weight loss—defined as weight loss of 5% of baseline body weight—after 1 year.5
These diets also affect cardiovascular risk. The Atkins and Zone diets both resulted in significantly increased high-density lipoprotein (HDL) cholesterol levels up to 12 months from baseline.5 Both also caused an early and significant reduction in triglycerides, while Zone dieters experienced a significant decrease in low-density lipoprotein (LDL) cholesterol.5
These diets also had effects on blood pressure—significantly reducing diastolic pressure. Atkins dieters, but not Zone dieters, also experienced a significant decrease in systolic pressure.5
A meta-analysis of numerous low-carbohydrate diets, not limited to Atkins, Zone, and South Beach, found modest improvements in systolic and diastolic blood pressure, plasma triglycerides, and HDL-cholesterol in obese subjects.6 Compared with low-fat diets, low-carbohydrate diets produced more significant reductions in total cholesterol, LDL-cholesterol, and triglycerides, along with an increase in HDL-cholesterol.7
The benefits of these individual fad diets remain questionable since long-term data is lacking. Note: Long-term data is available for generic low-carbohydrate diets and their relationship with cardiovascular risk. Cohort studies suggest that low-carbohydrate/high-protein diets are associated with significant cardiovascular8 and overall mortality rates.9 Further investigation reveals that among persons on a low-carbohydrate diet, those who consume most of their fat and protein from vegetable sources actually have lower cardiovascular and all-cause mortality rates,10 suggesting that carbohydrate consumption is only a piece of the puzzle.
It is important to realize that the low-carbohydrate diet bears implications for the diabetic patient or any patient concerned with control of blood glucose. The Atkins and Zone diets can reduce plasma insulin levels, and the Atkins diet can reduce fasting plasma glucose levels in the short term.5 A meta-analysis of obese patients on various low-carbohydrate diet protocols showed that significant reductions can be achieved in fasting plasma glucose, glycated hemoglobin, and plasma insulin.6
These findings, in addition to the benefits of low-carbohydrate diets (not high protein, high fat content) on markers of cardiovascular risk, it is evident that low-carbohydrate diets could be considered in the lifestyle modifications of patients with diabetes.
THE VEGETARIAN DIET
Vegetarian diets have long held cultural, religious and moral importance. The diet varies from lacto-ovo-vegetarianism (includes dairy and eggs) to veganism (excludes eggs, dairy, and other animal-based products). Individual diets that may allow meats or other animal products to varying degrees.11-13 Generally, vegetarian diets are characterized as lower in cholesterol and saturated fat, and higher in fiber, magnesium, potassium, vitamins C and E, folate, flavonoids, and other beneficial nutrients.10 Because of this composition, vegetarian diets offer certain health advantages—such as lower cholesterol levels and blood pressure, and reduced risk of heart disease, hypertension, and type 2 diabetes.10,12
Vegetarians, however, may be at risk for deficiency in vitamins B12 and D, iron, calcium, zinc, and long chain omega-3 fatty acids.10,11 Dietary deficiencies in vegetarians are not as common today as they were decades ago, mainly because of the availability of fortified products and meat substitutes, and a greater awareness of the need for balanced eating. It is important to stress careful and balanced diet planning to minimize the risk of deficiencies.10-12
An analysis of cohort studies revealed that vegetarians had a 24% reduction in mortality from heart disease vs. regular meat eaters.14 Furthermore, the greatest reduction in cardiovascular mortality was noticed in lacto-ovo-vegetarians and vegetarians who consumed fish.14 This highlights the importance of a diverse and balanced vegetarian diet.
The reduced cardiovascular mortality in vegetarians may be due to the lipid-lowering effects of their diets.11 Vegetarian diets also tend to be high in flavonoids and phytochemicals, which exert cardioprotective effects through inhibition of platelet aggregation and improvement in vascular endothelial function.11 Higher fiber consumption may also contribute to the superior lipid profile seen in vegetarians.10
Individuals following vegetarian diets are half as likely to develop diabetes versus non-vegetarians.15 For patients who already have diabetes, vegetarian diets might be effective in managing the disease. Vegetarian diets also result in improved insulin sensitivity and glycemic control, and a decrease in medication use.15 Possible explanations for these improvements include increased fiber intake, reduced glycemic index, reduced saturated fat intake, and weight loss with vegetarian diets.15 There are also psychological benefits for diabetic patients: A study of patients with type 2 diabetes randomized to follow a vegetarian diet demonstrated improved mood and quality of life, and decreased disinhibition and feelings of hunger.16
THE PALEOLITHIC DIET
The paleolithic diet is based on the idea that some of the most common health problems today—eg, CVD, type 2 diabetes and obesity—are so-called “diseases of civilization” and that the modern diet differs from the diet that the human body was designed to eat.17 By drawing on the diet and lifestyles of our hunter/gatherer ancestors, society can return to a state of health that predates the diseases of civilization.17
This diet emphasizes abundant consumption of vegetables, fruits, nuts, and meats (including bone marrow and internal organs), and prohibits dairy, legumes, and cereal grains, which did not become part of the human diet until the age of agriculture.18 So while other diets focus on the benefits of whole grains as a source of fiber and for glycemic control, the paleolithic diet advises no consumption of grains at all—encouraging fruits and vegetables as sources of carbohydrate and fiber instead.
Though current evidence weakly supports the idea that the paleolithic diet can prevent diseases of Western lifestyle,19 data from long-term randomized controlled trials are lacking. A 3-week study of healthy volunteers demonstrated significant short-term benefits including weight loss, reduction in waist circumference, and decreased systolic blood pressure.20 Those subjects, however, were also noted to be deficient in calcium under the study protocol.
Subjects consumed 36% less energy than prior to the study,20 suggesting that the paleolithic diet may promote satiety. In fact, one study found that the paleolithic diet is more satiating per calorie than a Mediterranean-like diet in patients with ischemic heart disease, even though the patients following the paleolithic diet consumed fewer calories per day.21
The diet also resulted in improved blood pressure and glucose tolerance, decreased insulin secretion, increased insulin sensitivity, and improved lipid profile,22 even in the absence of weight loss.18
THE GLUTEN-FREE DIET
The gluten-free diet is commonly prescribed in celiac disease, a condition in which patients are unable to tolerate gluten. Gluten is found in many grains, particularly wheat, and is responsible for providing elasticity to bread products. A gluten-free diet essentially eliminates most grains, but many other foods may innocuously contain gluten as an additive. Gluten-free formulations of common gluten-containing foods are becoming widely available.
Claims that a gluten-free diet can aid in weight loss have not yet been supported by medical evidence. On the contrary, there is evidence to show that patients with celiac disease gain weight upon starting a gluten-free diet; evidence is lacking in healthy subjects.23 Some gluten-free substitutes may actually contain as many calories as or more than their gluten-containing counterparts.23,24 Therefore, there would be no deficit in energy intake by eliminating gluten. In addition, the intake of whole grains and fiber is low in this diet.23
Anecdotal evidence that supports weight loss benefits from a gluten-free diet may be attributable to overall reduction in carbohydrates, particularly in refined carbohydrates. Research also shows that patients who follow a gluten-free diet are susceptible to deficiency in carbohydrate, iron, folate, niacin, and zinc.24 Some also point to gluten as being instrumental in contributing to colonic health and maintenance of blood pressure with increased consumption of whole grains.23
Recent animal studies show that a gluten-free diet can mediate inflammation, decrease adiposity gain, and reduce insulin resistance.25 Until these effects are demonstrated in humans, the gluten-free diet remains unsupported for weight loss or other health conditions aside from gluten sensitivity.
THE MEDITERRANEAN DIET
The Mediterranean diet is based not just on foods but also on the eating habits common to societies situated around the Mediterranean Sea.26 The diet is characterized by high consumption of fruits, vegetables, legumes, whole grains, and fish; moderate consumption of meats; olive oil as the main source of fat; and low-to-moderate consumption of red wine during meals.26
Epidemiological studies have shown an association between adherence to the Mediterranean diet and reduced risk of mortality and incidence of major chronic diseases.26,27 This diet is also associated with an improved biochemical profile and increased quality of life.26 The Mediterranean diet can prevent weight gain and has been shown to reduce the development of metabolic syndrome by 53%.28,29 A randomized trial comparing weight loss in persons who followed a Mediterranean diet, low-carbohydrate diet and low-fat diet revealed that metabolic benefits in addition to long-term weight loss were superior with the Mediterranean diet.30
There are also certain benefits to cardiovascular health. Primary prevention studies in the Greek population revealed that those with high adherence to the Mediterranean diet had a significant reduction in cardiovascular mortality—a 33% reduction in mortality corresponding to a 2-point higher score on a scale of diet adherence.27 Patients with previous myocardial infarction who began following the Mediterranean diet experienced a 73% reduction in the rate of coronary events and a 70% reduction in mortality vs. a control group after 27 months of follow-up.31
Compared to low-fat diets, the Mediterranean diet was associated with more favorable changes in body weight, body mass index, systolic pressure, diastolic pressure, fasting plasma glucose, total cholesterol, and C-reactive protein.32
The Mediterranean diet is also thought to be beneficial for patients with diabetes, since it emphasizes whole grains and high consumption of fruits and vegetables. A prospective cohort study demonstrated that after 4 years of follow-up, patients with high adherence to the Mediterranean diet had an 83% lower risk of developing diabetes.33 Randomized trials have also shown improvements in glycemic control, cardiovascular risk factors, and delay of antihyperglycemic therapy in patients following a Mediterranean diet.28
A meta-analysis of various dietary approaches to type 2 diabetes revealed that the Mediterranean diet resulted in a 0.47% reduction in glycated hemoglobin vs. a control diet, and had the largest effect size vs. other diets.34 While the Mediterranean diet has promising benefits, most Americans will not adopt the lifestyle of the Mediterranean diet over the long term.
THE AARP NEW AMERICAN DIET
A large prospective study of Americans over the last 25 years sought to delineate the effects of dietary and lifestyle choices not only on weight loss but also on cancer risk in the United States. The NIH-AARP Diet and Health Study found a reduction in colorectal cancer risk with whole grain consumption35 and a reduction in total cancer risk with calcium consumption.36 It also showed the association of diet with breast, kidney, and prostate cancer. The study has resulted in numerous publications, the findings of which were used to create the New American Diet.37
The AARP New American Diet promotes the idea of “diet” as a noun—something to live on, rather than something to go on. It suggests patients start to think of “food as medicine,” since food can impact every system of the body. The AARP New American diet focuses on consumption of water, whole grains and healthy fats, and dramatically reduces the intake of simple sugars and processed foods.37 Vegetables and fruits are recommended in high quantities. Fish, low-fat dairy, and moderate consumption of red meat are also prominent components.37
In addition, the New American Diet advises on eating behaviors, stressing that breakfast should not be skipped, meals and snacks should be eaten frequently (less food more often to prevent spikes in insulin levels), and meals should be eaten from a plate while sitting at a table.37 The diet does not require calorie counting.37
Since most patients have tried dieting at some point in their life, it is important for physicians to stay breast on the latest trends. Remember that lifestyle modification often has a more powerful and sustained effect on weight loss than prescription drugs, so physicians should provide guidance that is evidence-based, rather than anecdotal or fad-based.
Physicians should always counsel patients to make certain that food consumption is well balanced. Removing a particular nutrient or whole food group from a diet, or adopting an ancestral approach, leaves room for significant deficiencies in nutrition and health. Instead, care and thought should be put into dietary planning to ensure that patients are deriving benefits without concomitantly putting themselves at risk.
Physicians should advise patients on dietary adherence. A diet should not be a temporary change to eating habits to achieve a target weight or appearance; with this mindset, it is likely that a dieter will revert to previous eating patterns once that goal is achieved, and as a result, return to the previous weight and unhealthy state of being, and be skeptical of healthy eating. Instead, a healthy diet should be a long-term lifestyle change.
With dietary changes that are supported by evidence and through regular follow-up with primary care physicians, patients can expect to see profound improvements in their health status. Patients and physicians should work together to identify goals and select the most beneficial diet strategy to address weight and health problems. ■
References:
1.Smith AW, Borowski LA, Liu B, et al. US primary care physicians’ diet-, physical activity-, and weight-related care of adult patients. Am J Prev Med. 2011;41(1):33-42.
2.Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency, and knowledge. J Am Coll Nutr. 2008;27(2):287-298.
3.Kushner R. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546-552.
4.Ma Y, Pagoto SL, Griffith JA, et al. A dietary quality comparison of popular weight loss plans. J Am Diet Assoc. 2007;107:1786-1791.
5.Dansinger ML, Gleason JA, Griffith JL, et al. Comparison of the Ornish, Atkins, Weight Watchers, and Zone diets for weight loss and heart disease reduction: a randomized controlled trial. JAMA. 2005;293(1):43-53.
6.Santos FL, Esteves SS, da Costa Pereira A, et al. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev. 2012;13:1048-1066.
7.Hu T, Mills KT, Yao L, et al. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled trials. Am J Epidemiol. 2012;176(Suppl):S44-S54.
8.Trichopoulou A, Psaltopoulou T, Orfanos P, et al. Low carbohydrate high protein diet and long term survival in a general population cohort. Eur J Clin Nutr. 2007;61(5):575-581.
9.Lagiou P, Sandin S, Weiderpass E, et al. Low carbohydrate-high protein diet and mortality in a cohort of Swedish women. J Intern Med. 2007;261(4):366-374.
10.Fung TT, van Dam RM, Hankinson SE, et al. Low-carbohydrate diets and all-cause and all-cause specific mortality: two cohort studies. Ann Intern Med. 2010;153(5):289-298.
11.Position of the American Dietetic Association: Vegetarian Diets. J Am Diet Assoc. 2009;109:1266-1282.
12.Craig WJ. Nutrition concerns and health effects of vegetarian diets. Nutr Clin Prac. 2010;25(6):613-620.
13.McEvoy CT, Temple N, Woodside JV. Vegetarian diets, low-meat diets, and health: a review. Public Health Nutr. 2012;15(12):2287-2294.
14.Key TJ, Fraser GE, Thorogood M, et al. Mortality in vegetarians and non-vegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr. 1999;70(Suppl 3):S516-S524.
15.Barnard DA, Katcher HI, Jenkins DJA, et al. Vegetarian and vegan diets in type 2 diabetes management. Nutr Rev. 2009;67(5):255-263.
16.Kahleova H, Hrachovinova T, Hill M, Pelikanova T. Vegetarian diet in type 2 diabetes – improvement in quality of life, mood, and eating behavior. Diabet Med. 2013;30:127-129.
17.Eaton SB, Konner M. Paleolithic nutrition: a consideration of its nature and current implications. N Engl J Med. 1985;312:283-289.
18.Frassetto LA, Schloetter M, Mietus-Snyder M, et al. Metabolic and physiologic improvements from consuming a Paleolithic, hunter-gatherer type diet. Eur J Clin Nutr. 2009;63:947-945.
19.Lindeberg S. Paleolithic diets as a model for prevention and treatment of Western disease. Am J Hum Bio. 2012;24:110-115.
20.Osterdahl M, Kocturk T, Koochek A, Wandell PE. Effects of a short-term intervention with a Paleolithic diet in healthy volunteers. Eur J Clin Nutr. 2008;62(5):682-685.
21.Jonsson T, Granfeldt Y, Erlanson-Albertsson C, et al. A Paleolithic diet is more satiating per calorie than a Mediterranean-like diet in individuals with ischemic heart disease. Nutr Metab (Lond). 2010;7:85.
22.Jonsson T, Granfeldt Y, Ahrén B, et al. Beneficial effects of a Paleolithic diet on cardiovascular risk factors in type 2 diabetes: a randomized cross-over pilot study. Cardiovasc Diabetol. 2009;8:35.
23.Gaesser GA, Angadi SA. Gluten-free diet: imprudent dietary advice for the general population? J Acad Nutr Diet. 2012;112(9):1330-1333.
24.Marcason W. Is there evidence to support the claim that a gluten-free diet should be used for weight loss? J Am Diet Assoc. 2011;111(11):1786.
25.Soares FLP, de Oliveira Matoso R, Teixeira LG, et al. Gluten-free diet reduces adiposity, inflammation and insulin resistance associated with the induction of PPAR-alpha and PPAR-gamma expression J Nutr Biochem. 2013;24(6):1105-1111.
26.Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189-1196.
27.Trichopoulou A, Costacou T, Bamia C, Trichopoulou D. Adherence to Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599-2608.
28.Sofi F, Macchi C, Abbate R, et al. Mediterranean diet and health. BioFactors. 2013:1-8.
29.Kesse-Guyot E, Ahluwalia N, Lassale C, et al. Adherence to Mediterranean diet reduces the risk of metabolic syndrome: a 6-year prospective study. Nutr Metab Cardiovasc Dis. 2012;23(7):677-683.
30.Shai I, Schwarzfuchs D, Henkin Y, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008:359:229-241.
31.De Lorgeril M, Renaud S, Mamelle M, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454-1459.
32.Nordman AJ, Suter-Zimmermann K, Bucher HC, et al. Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors. Am J Med. 2011;124:841-851.
33.Martinez-Gonzalez MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ. 2008;336:1351-1358.
34.Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97:505-516.
35.Schatzkin A, Mouw T, Park Y, et al. Dietary fiber and whole-grain consumption in relation to colorectal cancer in the NIH-AARP Diet and Health Study. Am J Clin Nutr. 2007;85(5):1353-1360.
36.Park Y, Leitzmann MF, Subar AF, et al. Dairy food, calcium, and risk of cancer in the NIH-AARP Diet and Health Study. Arch Intern Med. 2009;169(4):391-401.
37.Whyte J. AARP New American Diet: Lose Weight, Live Longer. New Jersey: Wiley; 2013.

John Whyte, MD, MPH is a former medical advisor at the US Department of Health and Human Services in Washington, DC, and director of the Secretary’s Council on Private Sector Initiatives. He is currently the chief medical expert and vice president, health and medical education, at Discovery Channel in Silver Spring. He is also the author of AARP New American Diet: Lose Weight, Live Longer.


