Symptomatic Coagulase-negative Staphylococci Infections
A 3-week-old boy presented to our emergency department (ED) with a 1-day history of decreased urine output and oral intake. The boy was febrile, with a temperature of 39.5°C, though results of a physical examination were unremarkable. After a blood culture was drawn, the child’s mother left against medical advice. The next day, he was seen at an outside ED and was febrile. Blood cultures were again drawn, antibiotics were initiated, and he was transferred to our neonatal intensive care unit (NICU). Of note, the boy was born at 36 weeks gestation and mother’s prenatal history and laboratory results were unremarkable except for inadequately treated Group B streptococcus.
Upon admission to the NICU, he was febrile, tachypneic, tachycardic, and had 5 to 6 seizure-like episodes, for which he was treated with phenobarbital. Electroencephalogram (EEG) results obtained later that day showed diffuse neuronal dysfunction. Sepsis evaluation on the first day in the NICU revealed an elevated C-reactive protein level of 97 mg/L (reference range, 0-10 mg/L), a normal leukocyte count, and cerebrospinal fluid (CSF) studies suggestive of bacterial meningitis. CSF analysis included an elevated white blood cell count (nucleated cell count of 1169 with 82% neutrophils) (0% neutrophils), high protein levels of 270 mg/dL (reference range, 15-60 mg/dL), and glucose of 42 mg/dL (reference range, 50-80 mg/dL). The CSF culture grew rare oxacillin-sensitive Staphylococcus warneri.
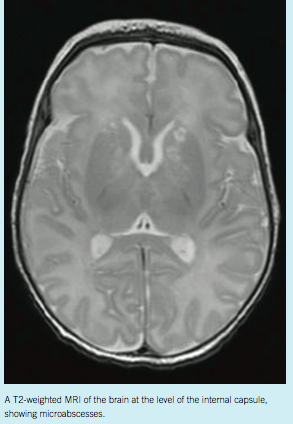
Blood cultures from both ED visits also returned positive for oxacillin-sensitive S hominis. Initial antibiotics were changed to oxacillin and cefotaxime to provide additional coverage for presumptive gram-negative bacteria. Two weeks into the NICU course, magnetic resonance imaging (MRI) was obtained due to the development of recurrent fevers despite targeted antibiotics. The imaging results showed microabscesses along the internal capsule and periventricular regions (Figure). By the end of 6 weeks of treatment, a repeat MRI showed significant improvement. At 9 weeks of age, the boy was discharged with unremarkable physical examination results and negative immunodeficiency studies.
DISCUSSION
Coagulase-negative staphylococci (CoNS) are found in normal skin flora and mucous membranes of humans and animals. CoNS infections typically occur in immunocompromised patients, particularly those with indwelling devices such as intravascular catheters.1 Neonates are vulnerable to these organisms due to both the high rate of invasive procedures they undergo and the ability of the bacteria to form biofilms.2 CoNS are responsible for one-third of nosocomial infections in NICUs in the United States.3 They are the most common microorganisms causing infections associated with health care in NICU neonates.4
S epidermidis comprises about 68% of CoNS infections isolated from cultures.3 Other clinically significant species include S saprophyticus and S lugdunensis. Rare species include S hominis, S haemolyticus, S capitis, S warneri, and S simulans. S hominis is the third most common organism recovered from neonates’ blood and from immunocompromised patients with bacteremia, septicemia, or endocarditis.5
CONCLUSION
It is challenging to differentiate CoNS bacteremia from contamination, especially without indwelling devices. We believe our patient had clinically significant bacteremia with meningitis because he was symptomatic, had positive blood cultures before antibiotics, and had a positive CSF culture with microabscesses on MRI. After treatment, repeat blood cultures were negative, and repeat MRI showed significant improvement, which supports that this was a true infection. To the best of our knowledge, this is the first case of brain microabscesses caused by CoNS in a neonate without indwelling devices. Thus, it is important to consider CoNS as a potential pathogen in a septic newborn without indwelling lines or invasive procedures.
Alexis Phillips, DO, is a third-year pediatric resident in the Department of Pediatrics at Children’s Hospital of Michigan in Detroit.
Nischala Rajegowda, MD, and Beena Sood, MD, are with the Department of Pediatrics in the division of Neonatal and Perinatal Medicine at Children’s Hospital of Michigan and Hutzel Womens Hospital in Detroit.
REFERENCES
1. Hyun DY. Coagulase-negative staphylococcal Infections. In: Feigin MD, Ralph D, Cherry J, Demmler-Harrison GJ. Feigin and Cherry’s Textbook of Pediatric Infectious Diseases. 7th ed. Philadelphia, PA: Saunders; 2013: 1131-1140.
2. Hira V, Sluijter M, Goessens WH, et al. Coagulase-negative staphylococcal skin carriage among neonatal intensive care unit personnel: from population to infection. J Clin Microbiol. 2010;48(11):3876-3881.
3. Cimiotti JP, Hass JP, Della-Latta P, Wu F, Saiman L, Larson L. Prevalence and clinical significance of Staphylococcus warneri in the neonatal intensive care unit. Infect Control Hosp Epidemiol. 2007; 28(3):326-330.
4. Sohn AH, Garrett DO, Sinkowitz-Cochran RL, et al. Prevalence of nosocomial infections in neonatal intensive care unit patients: Results from the first national point-prevalence survey. J Pediatr. 2001;139(6):821-827.
5. Mendoza-Olazarán S, Morfin-Otero R, Rodríguez-Noriega E, et al. Microbiological and molecular characterization of Staphylococcus hominis isolates from blood. PLoS ONE. 2013;8(4):e61161.


