Rhizopus Infection
A 64-year-old man with a past medical history of chronic myelogenous leukemia had an allogeneic stem cell transplant 2 years prior. However his leukemia had relapsed and had subsequently transformed into acute mylogenous leukemia. He then underwent a second allogeneic stem cell transplant using a new donor.
His immediate post-transplant in-hospital course was well tolerated. He had received graft-versus-host-disease immunosuppression with cyclosporine and methotrexate and was discharged home on cyclosporine and antimicrobial prophylaxis with sulfamethoxazole-trimethoprim, acyclovir, and voriconazole.
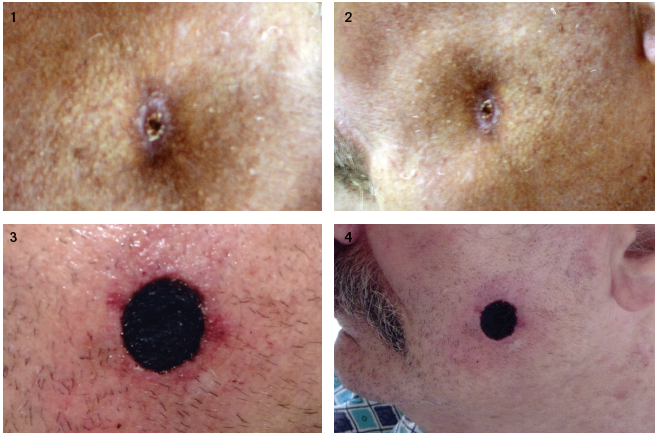
One month after discharge, the patient began developing fevers. He was admitted for further evaluation and placed on broad-spectrum antibiotics and continued on voriconazole. When fevers persisted, antibiotics were changed and voriconazole was switched to amphotericin. During his hospital stay, over the course of a week, he had begun to develop a plaque-like lesion on his left cheek (Figures 1 and 2). The area was non-tender.
The infectious disease consult was concerned for a fungal infection and the area was excised. Microbiology, based on the appearance of its bread hyphae with septations, identified the genus Rhizopus. Rhizopus is a member of the order of fungal infections known as Mucorales.
After the excision of the lesion on his left cheek, the area began to appear necrotic—a hallmark of the infection (Figures 3 and 4). He was switched from amphotericin to posaconazole, which has shown activity against the fungus.
Ultimately, the patient developed pneumonia. Due to his overall worsening clinical picture, the patient chose not to undergo bronchoscopy which would have necessitated intubation, and died after transitioning to comfort care. No autopsy was performed.
Mucorales are being recognized as emerging life-threatening infections, particularly in diabetic and immunocompromised patients. Voriconazole, a common antifungal therapy of the azole class, is used for prophylaxis against Aspergillus and Candida species in immunocompromised patients. However, it offers limited protection against Mucorales.1 Unusual or rapidly growing skin lesions in diabetics or immunocompromised patients such as transplant recipients should be expeditiously evaluated.2 While the use of amphotericin may be considered the front line therapy, the use of another azole—posaconazole—may be recommended, particularly in refractory cases. ■
Amir Steinberg, MD, shares his first-hand account of the case here:References:
1.Lagner S, Staber PB, Neumeister P. Posaconazole in the management of refractory fungal infections. Ther Clinical Risk Manag. 2008;4(4):747-757.
2.Lekakis LJ, Lawson A, Prante J, et al. Fatal rhizopus pneumonia in allogeneic stem cell transplant patients despite posaconazole prophylaxis: two cases and review of the literature. Biol Blood Marrow Transplant. 2009;15(8):991-995.


