A Girl With Cerebriform Palmar Plaques
Case In Point
An Intriguing Diagnosis
A 6-month-old African American girl first presented to the dermatology clinic at Children’s Medical Center of Dallas for large birthmarks. Since birth, these marks had gradually enlarged and thickened, without apparent tenderness or skin breakdown. There was no family history of similar lesions, large birthmarks, or skin cancer. The girl was alert and interactive without abnormal facies or known developmental delay.

Physical examination at the time was notable for cerebriform hyperplasia on the palms bilaterally (Figure 1). Dark brown macules and pebbly plaques of varied thickness were noted over large portions of the upper and lateral back, extensor arms, and chest, in a geographic distribution (Figure 2). She also had dark brown and bluish macules on the lower abdomen, inguinal area, arms, and legs. Some of the areas had associated hypertrichosis. Soft dermal plaques altered her arm circumference roughly symmetrically.
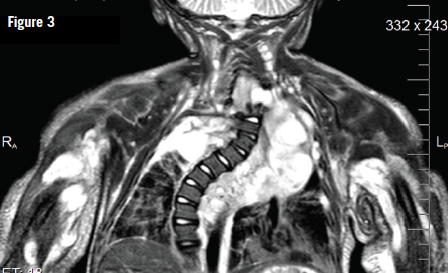
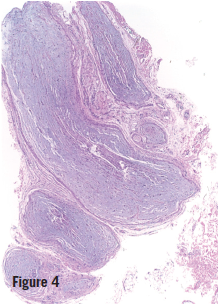
Later, when the girl was 10 months old, a biopsy specimen of the skin of her left palm showed neurofibroma; a biopsy specimen of a brown plaque on her back showed plexiform neurofibroma (Figure 3). Magnetic resonance imaging (MRI) scans, with and without contrast, of her chest and abdomen showed multiple infiltrative masses in the neck, chest, and upper extremities, which initially were read as being consistent with venous malformations; later, in conjunction with other studies, these were reinterpreted as being consistent with internal neurofibromas (Figure 4). The girl received a diagnosis of neurofibromatosis type 1 (NF1). She was referred to the multidisciplinary Comprehensive Neurofibromatosis Clinic at Children’s Medical Center of Dallas.

A more recent MRI has shown further progression of the extensive plexiform neurofibromas; most concerning is extension into the intraspinal cervical region with resultant severe compression of the spinal cord. Extensive plexiform neurofibromas of the subglottic and intrathoracic trachea with narrowing and dystrophic scoliosis also have been noted. At 2 years of age, the girl has been admitted to the hospital intensive care unit twice for respiratory distress attributed to the narrowing of her airways in combination with medications such as anesthesia and chemotherapeutics. She is currently stable on bilevel positive airway pressure therapy.
DISCUSSION
The clinical differential diagnoses for this patient included Proteus syndrome, Cowden syndrome, other systematized epidermal nevus syndromes, melanocytic nevi, and NF1.
The cerebriform appearance of the palms, the dark brown plaques resembling large connective-tissue nevi, and the altered circumference of the girl’s arms were clinically suggestive of Proteus syndrome; however, the plexiform and subcutaneous neurofibromas also led to the initial consideration of NF1.1 The presence of numerous café au lait macules also favored a diagnosis of NF1.
 Typically, plexiform neurofibromas are considered to be a finding more common outside of infancy. This case illustrates a unique presentation of NF1 and the importance of clinical-pathologic correlations in establishing diagnoses. Including Proteus syndrome in differential diagnosis might have influenced how the MRI scans were interpreted initially, since upon reassessment after biopsies, the concern shifted from venous malformations to internal plexiform neurofibromas.
Typically, plexiform neurofibromas are considered to be a finding more common outside of infancy. This case illustrates a unique presentation of NF1 and the importance of clinical-pathologic correlations in establishing diagnoses. Including Proteus syndrome in differential diagnosis might have influenced how the MRI scans were interpreted initially, since upon reassessment after biopsies, the concern shifted from venous malformations to internal plexiform neurofibromas.
Among the diagnostic criteria for Proteus syndrome, cerebriform connective tissue nevi—especially on the soles of the feet even more so than the palms—are almost pathognomonic.2 However, as in our case, NF1 can also be protean in nature, mimicking other disorders. Large and extensive cutaneous plexiform neurofibromas may be associated with comorbid internal lesions, which, depending on their location, can be life threatening; therefore, imaging to assess for such internal lesions is recommended.
REFERENCES:
1. Happle R. The group of epidermal nevus syndromes: part I. Well defined phenotypes. J Am Acad Dermatol. 2010;63(1):1-22.
2. Nguyen D, Turner JT, Olsen C, Biesecker LG, Darling TN. Cutaneous manifestations of Proteus syndrome: correlations with general clinical severity. Arch Dermatol. 2004;140(8):947-953.


