Diffuse Cerebral Fat Emboli in Fat Embolism Syndrome
AUTHORS:
Sukhwinder Johnny S. Sandhu, MD; Austin Fischer, DO; Patrick Natter, MD; Dinesh Rao, MD; Inbal Cohen-Rasen, MD; Paul L. Wasserman, DO; and Dalys E. Haymes, MD
AFFILIATION:
University of Florida College of Medicine, Jacksonville, Florida
CITATION:
Sandhu SJS, Fischer A, Natter P, Rao D, Cohen-Rasen I, Wasserman PL, Haymes DE. Diffuse cerebral fat emboli in fat embolism syndrome. Consultant. 2017;57(3):187-188.
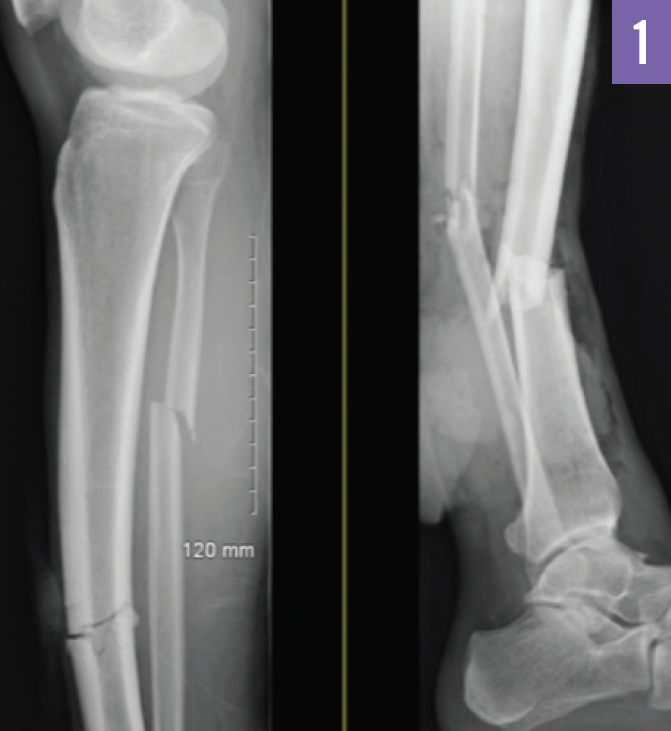
A 31-year-old man was admitted to the emergency department (ED) following a motor vehicle accident in which he had sustained multiple bilateral long-bone fractures of the lower extremities. These included fractures of the right distal tibia and the right proximal fibula, as well as open fractures of the left tibia and left fibula (Figure 1).
At presentation, the patient had an initial Glasgow coma scale (GCS) score of 11 of 15 (correlating with moderate brain injury) but decompensated to a GCS score of 6 (correlating with severe brain injury). He was hemodynamically unstable. The results of an initial computed tomography (CT) scan of the head were unremarkable. The patient underwent surgical repair of the fractures. After surgery, he was stable and following commands, with neurovascular checks being performed every hour.
On day 2, the patient developed tachycardia, anemia, thrombocytopenia, and a fever. Physical examination demonstrated posturing, an inability to follow commands, and a lack of eye opening. A second CT scan of the head revealed no acute change. Diffusion-weighted magnetic resonance imaging (MRI) of the brain showed extensive punctate areas of restricted diffusion diffusely involving the deep white matter, gray-white interface, basal ganglia, splenium, and corpus callosum (Figure 2). An echocardiogram showed no evidence of a right-to-left interatrial shunt.
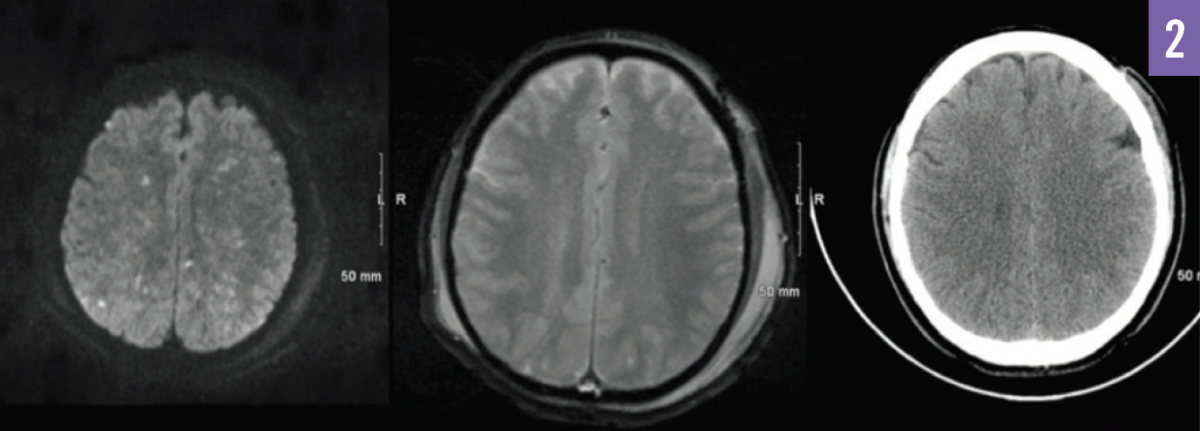
Figure 2. Diffusion-weighted MRI (left); gradient echo MRI, with lesions not visualized (middle); and CT, with lesions not visualized (right).
Susceptibility-weighted MRI 2 days later showed numerous punctate foci of susceptibility effect throughout the superficial and deep white matter, genu, splenium, midbrain, pons, and bilateral cerebellar hemispheres (Figure 3). The patient’s mental status slowly improved over time, with his GCS score reaching 14 on day 48.

Figure 3. Fluid-attenuated inversion recovery MRI (left); susceptibility-weighted MRI (middle); and diffusion-weighted MRI (right).
Discussion. This patient presented with findings that were suggestive of cerebral fat emboli (CFE) in fat embolism syndrome (FES). The more complex and potentially deadly FES occurs in 0.9% to 2.2% of cases of traumatic long-bone fractures as a result of the release of fatty intramedullary contents into the venous circulation.1,2 The deformable fat globules can traverse the pulmonary circulation, reaching the systemic circulation, and can cause embolic showers.3 Symptoms can be immediate, occurring within 48 hours in 85% of cases. However, the syndrome may be delayed up to 3 days following trauma.3
Gurd and Wilson4 originally proposed diagnostic criteria for FES that included 1 major feature and 4 minor features. The major criteria are hypoxia, decline in mental status, and petechial rash. The minor criteria are fever, tachycardia, retinal changes, jaundice, renal insufficiency, anemia, thrombocytopenia, elevated erythrocyte sedimentation rate, and fat macroglobulinemia.2,4,5
Since most patients will become symptomatic within 48 hours, the diagnosis of FES has shifted to include neuroimaging.5 Cerebral CT scan findings are usually normal.2 MRI of the brain using T2-weighted, diffusion-weighted, gadolinium contrast-enhanced, and susceptibility-weighted imaging has improved the diagnosis of CFE.6 On T2-weighted MRI images, a characteristic “starfield” pattern of multiple small, scattered, and hyperintense intracerebral lesions is seen.2,7,8 On diffusion-weighted images, scattered foci of restricted diffusion are seen. On susceptibility-weighted images, punctate foci representing microhemorrhage are seen predominantly in the white matter.6 The main differential diagnosis is diffuse axonal injury, which predominantly occurs at the gray-white matter interface of the frontotemporal lobes and corpus callosum.6
Treatment. Supportive care can lead to resolution of FES. The mainstay of therapy is oxygen administration and mechanical ventilation to maintain tissue oxygenation.3 Echocardiography should also be performed, given that the presence of an intracardiac shunt may also contribute to fat emboli in the systemic circulation.7 Inconclusive evidence exists to recommend heparin or corticosteroids to treat FES.3
Early fracture fixation and minimizing patient transport can decrease the occurrence of complications following long-bone trauma.3 Continuous pulse oximetry monitoring may detect early pulmonary symptoms resulting from fat emboli. Administering 10 mg of methylprednisolone every 8 hours starting in the ED may be beneficial in patients who are at significant risk for developing FES.3
With supportive care, the mortality rate for FES is less than 10%.1 It is beneficial to monitor the patient’s GCS score. Also, the number of punctate lesions noted on brain MRI scans has correlated inversely with the GCS score.2 Most case reports of CFE show reversal of neurologic symptoms within 10 days of admission.1,2,9 However, brain atrophy and demyelination have been reported as late changes.6 The starfield pattern on MRI images is commonly associated with a favorable prognosis.1 Resolution of the punctate lesions should occur in a few weeks to a few months.2
References:
- Aravapalli A, Fox J, Lazaridis C. Cerebral fat embolism and the “starfield” pattern: a case report. Cases J. 2009;2:212.
- Parizel PM, Demey HE, Veeckmans G, et al. Early diagnosis of cerebral fat embolism syndrome by diffusion-weighted MRI (starfield pattern). Stroke. 2001;32(12):2942-2944.
- Richards RR. Fat embolism syndrome. Can J Surg. 1997;40(5):334-339.
- Gurd AR, Wilson RI. The fat embolism syndrome. J Bone Joint Surg Br. 1974;56B(3):408-416.
- Kellogg RG, Fontes RBV, Lopes DK. Massive cerebral involvement in fat embolism syndrome and intracranial pressure management: case report. J Neurosurg. 2013;119(5):1263-1270.
- Kuo K-H, Pan Y-J, Lai Y-J, Cheung W-K, Chang F-C, Jarosz J. Dynamic MR imaging patterns of cerebral fat embolism: a systematic review with illustrative cases. AJNR Am J Neuroradiol. 2014;35(6):1052-1057.
- Gregorakos L, Sakayianni K, Hroni D, et al. Prolonged coma due to cerebral fat embolism: report of two cases. J Accid Emerg Med. 2000;17(2):144-146.
- Walshe CM, Cooper JD, Kossmann T, Hayes I, Iles L. Cerebral fat embolism syndrome causing brain death after long-bone fractures and acetazolamide therapy. Crit Care Resusc. 2007;9(2):184-186.
- Ryu CW, Lee DH, Kim TK, et al. Cerebral fat embolism: diffusion-weighted magnetic resonance imaging findings. Acta Radiol. 2005;46(5):528-533.


