Peer Reviewed
Tracheal Perforation, a Life-Threatening Complication of Endotracheal Intubation
Authors:
Jiesu L. Sun, MD, MPH
Department of Internal Medicine, Baylor University Medical Center, Dallas, Texas
Helen Hashemi, MD
Department of Internal Medicine, Baylor University Medical Center, Dallas, Texas
Ginger Tsai-Nguyen, MD
Department of Pulmonary and Critical Care Medicine, Baylor University Medical Center, Dallas, Texas
Adan Mora Jr, MD
Department of Pulmonary and Critical Care Medicine, Baylor University Medical Center, Dallas, Texas
Citation:
Sun JL, Hashemi H, Tsai-Nguyen G, Mora A Jr. Tracheal perforation, a life-threatening complication of endotracheal intubation [published online October 28, 2019]. Pulmonology Consultant.
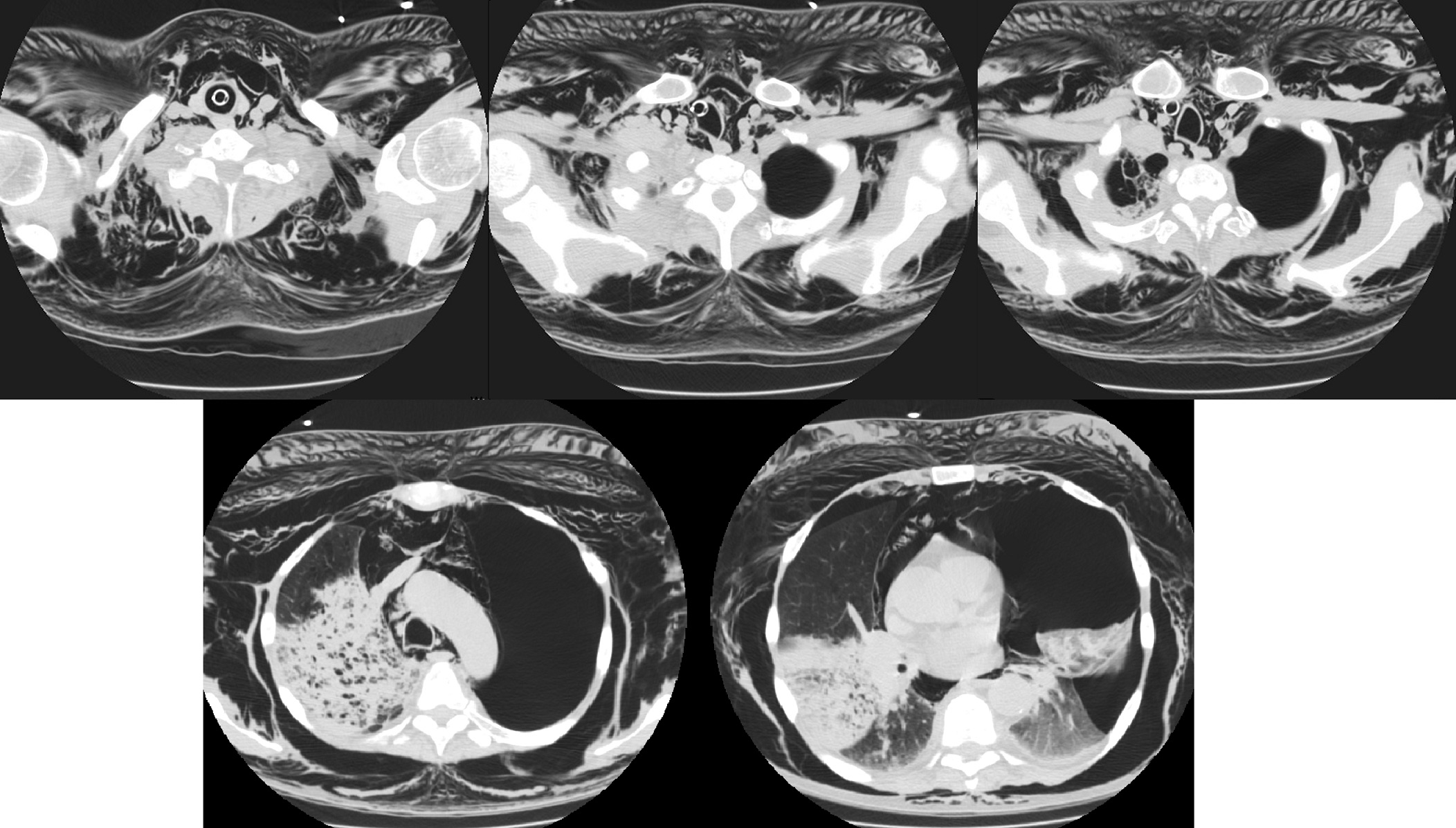
A 62-year-old man with metastatic prostate cancer, congestive heart failure, and chronic obstructive pulmonary disease (COPD) presented to an outside emergency department (ED) with right-sided chest pain and dyspnea. The patient’s initial chest radiographs showed consolidation of the right upper lobe, a finding concerning for pneumonia (Figure 1). Additional computed tomography (CT) scans of the chest also suggested right upper lobe pneumonia.

While at the outside ED, the patient became tachypneic and hypoxic. Initial efforts at noninvasive ventilation with bronchodilator treatment proved insufficient, and the patient underwent rapid sequence intubation. He was intubated on the second attempt via video laryngoscopy with a 7.0-mm endotracheal tube (ETT). Records noted that the intubation was “difficult with resistance.”
After the intubation, the patient was noted to have significant subcutaneous emphysema in the neck, chest, and abdomen. Breath sounds were difficult to hear, but the patient’s oxygenation and ventilation were acceptable.
Repeated CT scans of the chest revealed that the tip of the ETT had perforated the right anterolateral aspect of the trachea with extension into the mediastinum, leading to severe pneumomediastinum, subcutaneous emphysema, and a large left-sided tension pneumothorax (Figure 2).
A left-sided chest tube was placed, and broad-spectrum antibiotics were administered. The patient gradually became hypotensive and required norepinephrine after inadequate response to fluids. He was subsequently emergently flown to a tertiary center for higher-level care.
Upon arrival to the intensive care unit at the tertiary center, the patient was hypotensive, with mean arterial pressures in the 40 to 50 mm Hg range, despite administration of additional fluids and rapid escalation to maximal norepinephrine, phenylephrine, and vasopressin dosing. Eventually, a pulse was no longer palpable or heard on Doppler ultrasonography.
Multiple code blues ensued, with placement of bilateral large-bore chest tubes for treatment of bilateral pneumothoraxes and a right-sided hemothorax. Despite aggressive resuscitation measures, the patient died.
DISCUSSION
Airway management is a primary life-saving procedure. Endotracheal intubation is the most commonly used method of securing the airway in the inpatient setting and out of the hospital.1 The most common indications for tracheal intubation are acute respiratory failure, airway protection in patients with altered mental status, and general anesthesia for an operation.2 Complications of endotracheal intubation include throat pain, laryngitis, mucosal ulceration, laryngeal or tracheal stenosis, aspiration, esophageal intubation, bronchial intubation, atelectasis, and tracheal rupture.3 Tracheal perforation is a rare complication of endotracheal intubation.4
Tracheal perforation is rare, with an overall occurrence rate of 0.05% to 0.37%, and is most commonly associated with head and neck injury.5 Iatrogenic rupture is rare and usually is a complication of endotracheal intubation, occurring in approximately 1 in 20,000 intubations.4 Risk factors for intubation-associated rupture include multiple forced intubation attempts, inexperience of the health care professional, ETT introducers that protrude beyond the tube’s tip, repositioning of the ETT without deflation of the cuff, inappropriate ETT sizing, use of a double-lumen ETT, and movements of the patient’s head.5,6
The most common reported presentation is subcutaneous emphysema, followed by pneumomediastinum, pneumothorax, hemoptysis, and dyspnea; rarely does tracheal perforation progress to pneumopericardium and shock.5 Often, the diagnosis is delayed because of the nonspecific symptoms. While CT scans can provide evidence of air leak into the mediastinum and detect pneumothorax, these scans have only 85% sensitivity for detecting tracheal injury.7 Bronchoscopy is the mainstay for diagnosis of a tracheal tear.8
No consensus or clear guidelines exist on the management of tracheal perforations. However, management has trended toward a more conservative approach in patients with minimal and nonprogressive symptoms, with no air leakage, with no respiratory difficulty, with no esophageal injury, who are spontaneously breathing, and in whom extubation is expected within 24 hours.8 Broad-spectrum antibiotics should be administered given the that mediastinitis is one of the more significant possible complications of tracheal perforation.7 Tracheostomy below the site of tear can be performed to reduce intratracheal pressure and leak through the tear, allowing for spontaneous healing.7,10 Surgical repair is more common if the lesion is greater than 2 cm; this can entail direct intraluminal suturing of proximal tracheal lacerations or tracheal stenting.7,11
The mortality rate of tracheal perforation was found to be 22% in a systematic literature review of 182 cases.5
Tracheal perforation is an uncommon complication of endotracheal intubation that can lead to life-threatening consequences. Early diagnosis is essential for the implementation of appropriate interventions.
REFERENCES:
- Wang HE, Szydlo D, Stouffer JA, et al; ROC Investigators. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Resuscitation. 2012;83(9):1061-1066.
- Ezri T, Warters RD. Indications for tracheal intubation. In: Hagberg CA, ed. Benumof's Airway Management: Principles and Practice. 2nd ed. Philadelphia, PA: Mosby Elsevier; 2007:chap 15.
- Thompson DS, Read RC. Rupture of the trachea following endotracheal intubation. JAMA. 1968;204(11):995-997.
- Chang C-Y, Cheng S-L, Chang S-C. Conservative treatment of severe tracheal laceration after endotracheal intubation. Respir Care. 2011;56(6):861-862.
- Miñambres E, Burón J, Ballesteros M, Llorca J, Muñoz P, González-Castro A. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg. 2009;35(6):1056-1062.
- Lampl L. Tracheobronchial injuries. Conservative treatment. Interact Cardiovasc Thorac Surg. 2004;3(2):401-405.
- Chen J-D, Shanmuganathan K, Mirvis SE, Killeen KL, Dutton RP. Using CT to diagnose tracheal rupture. Am J Roentgenol. 2001;176(5):1273-1280.
- Hasan A, Low DE, Ganado AI, Norton R, Watson DCT. Tracheal rupture with disposable polyvinylchloride double-lumen endotracheal tubes. J Cardiothorac Vasc Anesth. 1992;6(2):208-211.
- Óvári A, Just T, Dommerich S, et al. Conservative management of post-intubation tracheal tears—report of three cases. J Thorac Dis. 2014;6(6):E85-E91.
- Mullan GPJ, Georgalas C, Arora A, Narula A. Conservative management of a major post-intubation tracheal injury and review of current management. Eur Arch Otorhinolaryngol. 2007;264(6):685-688.
- Cardillo G, Carbone L, Carleo F, et al. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg. 2010;37(3):581-587.


