Four Cases of Bone Disorders

Congenital Absence of Carpal Navicular Bone
After a galley door slammed shut on his right wrist, a 37-year-old deckhand sought medical attention. He had no history of previous injury to the wrist. On examination, he had 50% of normal range of motion, and there was palpable tenderness and bony swell-ing at the dorsum of the wrist.
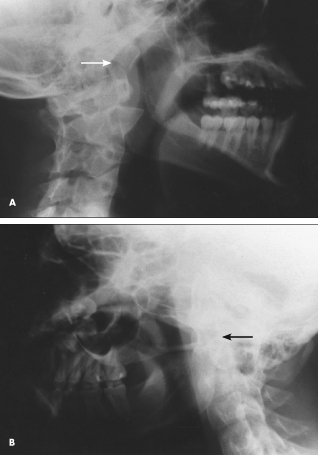
An x-ray film (A) was surprising: it showed absence of the navicular bone, secondary degenerative changes primarily in the capitate and lunate bones, extreme atrophy of the radial styloid, and a deformed radial articular surface with an almost transverse orientation of the radiocarpal joint. Normal bone structure is shown for comparison (B).
Absence of the carpal navicular bone is rare. In most of these patients, there are congenital malformations in other body systems as well, and a “VATER” syndrome is found in some.1 This consists of three or more of the following malformations: vertebral defects; anal atresia; tracheo-esophageal fistula; and renal and radial dysplasia.
REFERENCE:
1. Treble NJ. Congenital absence of the scaphoid in the ‘VATER’ association. J Hand Surg [Br]. 1985;10:251-252.
(Case and films courtesy of Drs Robert P. Blereau and Timothy Haley.)
____________________________________________________________________________________________________________________________________________

Post-Traumatic Osteoarthritis
A 65-year-old man experienced a hard fall 40 years ago, when he was a paratrooper: he landed on his right
leg and sustained trauma to the right hip. This current radiograph demonstrates a striking example of advanced hypertro-phic degenerative osteoarthritic changes of the right hip.
This condition is post-traumatic osteoarthritis (disruptive articular trauma), an uncommon form of second-ary osteoarthritis. The typical findings, illustrated here, include marked narrowing of the joint space, large osteophytes extending from the femoral head and the acetabulum (particularly from the superior
aspect), and slight compression of the femoral head. In contrast, the radiologic appearance of the left hip is unremarkable for the patient’s chronologic age.
Unfortunately, most cases of post-traumatic osteo-arthritis are not so clear-cut. To establish the diagnosis, the following findings are necessary:
•The history relates a specific, definable trauma, such as an automobile accident, beating, or crush injury.
•An effusion or structural damage occurred following the injury.
•Similar disease is not present in nontraumatized joints.
Additional points that favor the diagnosis of post-traumatic osteoarthritis include monarticular or pauciarticular involvement; significant arthritis in a joint that is not usually affected (eg, ankle, wrist, elbow, or metacarpophalangeal joint); and radiographic evidence of healed fractures or foreign bodies near the joint in question.
General exposure to heat or cold, hard work, or malnutrition may contribute to degenerative arthritis. However, these factors are not likely to produce post-traumatic osteoarthritic changes. This diagnosis refers to a localized process.
(Case and film courtesy of Dr William P. Skelton III.)
_________________________________________________________________________________________________________________
Bilateral Mandibular Fractures
A 20-year-old man sustained a 2- to 3-cm soft-tissue laceration in the middle of the chin when he fell, face forward, onto pavement. He reported left preauricular pain with limited opening of his mouth and a change from his normal bite. Examination showed a mild anterior open bite and limited opening. A mandibular film series, consisting of anteroposterior, lateral right (A), left lateral oblique (B), and reverse Towne’s (C) views, demonstrated a left subcondylar fracture. Because of the type of fall and resulting soft-tissue injuries, a pan-o-ramic radiograph was obtained (D). The film demonstrated a bilateral fracture.
A direct anterior blow often results in bilateral subcondylar fractures with midline soft-tissue damage and anterior open bite, as was found in this case. The lacerations were closed, and elastic intermaxillary fixation was carried out on the fractures. The patient subsequently had good occlusion and full range of motion.
(Case and films courtesy of Dr Richard Schell.)
____________________________________________________________________________________________________________________________
Acute Renal Osteodystrophy
 This x-ray film of a man in his 50s illustrates an extreme case of renal osteodystrophy. On examination, the patient’s legs were very tender and one could actually see the femur bend in the examiner’s hands as if it had a greenstick fracture. The patient, who was on dialysis, had features of severe malnutrition and proximal myopathy despite prolonged hospitalization. He died a few weeks after this film was taken.
This x-ray film of a man in his 50s illustrates an extreme case of renal osteodystrophy. On examination, the patient’s legs were very tender and one could actually see the femur bend in the examiner’s hands as if it had a greenstick fracture. The patient, who was on dialysis, had features of severe malnutrition and proximal myopathy despite prolonged hospitalization. He died a few weeks after this film was taken.
The clinical picture of renal osteodystrophy varies from extreme osteomalacia and demineralization (as in this patient) to states of markedly increased bone turnover (as in hyperparathyroidism). Additional conditions that affect bone metabolism, such as immobilization, can further exacerbate the disorder. Aluminum-related bone disease and encepha-lopathy are common in patients who have renal dysfunction.
(Case and film courtesy of Dr Jamil A. Kirdar.)


