Peer Reviewed
Recurrent Tubo-Ovarian Abscess in a Nonsexually Active Adolescent
AUTHORS:
Darla Fink, MD1 • Peter Paul C. Lim, MD2 • Ankita Desai, MD2 • Allayne B. Stephans, MD3 • Michael A. Wien, MD4
AFFILIATIONS:
1Department of Pediatrics, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, Ohio
2Department of Pediatric Infectious Diseases, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, Ohio
3Department of Pediatric Hospital Medicine, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, Ohio
4Department of Pediatric Radiology, University Hospitals Rainbow Babies and Children’s Hospital, Cleveland, Ohio
CITATION:
Fink D, Lim PPC, Desai A, Stephans AB, Wien MA. Recurrent tubo-ovarian abscess in a nonsexually active adolescent. Consultant. 2022;62(1):e26-e28. doi:10.25270/con.2021.04.00010
Received December 20, 2020. Accepted January 29, 2021. Published online April 21, 2021.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Darla Fink, MD, University Hospitals Rainbow Babies and Children’s Hospital, Department of Pediatrics, 11100 Euclid Avenue, Cleveland, OH 44106 (Darla.Fink@UHhospitals.org)
An 11-year-old girl presented to our emergency department with a 3-day history of left lower abdominal pain, blood-streaked emesis, and anorexia. She denied history of fever, weight loss, diarrhea, dysuria, or vaginal discharge.
Her medical history is significant for nighttime enuresis and obesity. Menarche had started 6 months prior to presentation, and she reported that her cycles were irregular. The patient was interviewed with and without her caregiver present by the primary care team and social workers, but it did not identify any evidence of oral, anal, or vaginal intercourse. Her family history was noncontributory.
Physical examination. The patient was afebrile (37.3 °C) and obese, with a body mass index of 30 kg/m2. Her abdomen was soft, with tenderness in the bilateral lower quadrants. Results of a complete blood cell count revealed normal levels of white blood cells, hemoglobin, hematocrit, and platelets. However, her level of neutrophils was high at 78%, and her C-reactive protein level was elevated at 10.56 mg/dL. A urine pregnancy test was negative. Results of a urinalysis showed a moderate leukocyte esterase level and 77 white blood cells and was negative for nitrites. A urine culture was positive for mixed urethral flora.
A pelvic ultrasonography scan showed a dilated, blind-ended, fluid-filled tubular structure in the right lower abdomen, which raised suspicion for appendicitis (Figure 1). A pediatric surgeon was consulted, and a computed tomography scan was performed, results of which showed a heterogenous complex lesion within the lower abdominal mesentery. Magnetic resonance imaging (MRI) of the abdomen and pelvis revealed a hydrosalpinx with thick peripheral enhancement, raising suspicion for superimposed infection and inflammation, as well as an arcuate uterus (Figure 2).


Figure 1. Transverse (A) and sagittal (B) views of the ultrasonography scans of the pelvis demonstrated a thick-walled hypoechoic, nonvascular, tubular structure containing internal debris in the left lower abdomen. It is separate from the bowel and bladder, suggestive of pyosalpinx (arrows).


Figure 2. Coronal (A) and axial (B) T1 postcontrast, fat-saturated, maximum-intensity-projection MRI scans were performed of the abdomen and pelvia within 24 hours of the ultrasonography scans in Figure 1. Results demonstrated a thick-walled, blind-ending, tubular structure in the left lower quadrant that was anterosuperior to the uterus (asterisk). These scans confirmed a dilated, tortuous, fluid-filled fallopian tube (arrows).
Diagnostic laparoscopy was also performed, results of which revealed a large adnexal fluid collection consistent with tubo-ovarian abscess. Intraoperatively, a gynecologist performed a pelvic washout. A peritoneal culture grew Streptococcus bovis and Bacteroides thetaiotaomicron. Chlamydial and gonorrhea cultures taken from the patient’s pelvic fluid and urine nucleic acid amplification testing (NAAT) results were negative. Test results for HIV, hepatitis B and C viruses, and syphilis were also negative. The patient’s fecal calprotectin and hemoglobin A1c levels were also within normal limits.
The patient was empirically started on cefoxitin, 2000 mg, and doxycycline, 100 mg, every 6 hours, and then ampicillin/sulbactam, 2000 mg, every 6 hours per culture susceptibility results. She was discharged home with amoxicillin/clavulanic acid to complete a 14-day course.
Approximately 1 month later, the patient followed up for a repeat pelvic ultrasonography scan, which showed a reaccumulation of pelvic fluid in the area of the previous left tubo-ovarian abscess (Figure 3). Repeat laboratory studies showed a persistent elevation in C-reactive protein level of 9.38 mg/dL. She was readmitted to the hospital and underwent drainage of pelvic fluid by an interventional radiologist, which revealed a left-sided tubo-ovarian abscess. Results of a fluoroscopy raised concern for a noncommunicating left uterine horn. However, a repeat pelvic MRI did not show evidence of a noncommunicating left uterine horn. A repeat peritoneal fluid culture grew Bacteroides thetaiotaomicron. This time, the patient received ampicillin/sulbactam, 2000 mg, every 6 hours and was discharged with amoxicillin, 875 mg, and clavulanic acid, 12 mg, every 12 hours to complete another 14-day course. She was also placed on an oral contraceptive.
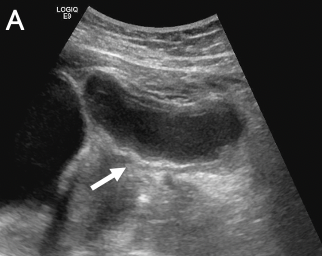

Figure 3. Transverse (A) and sagittal (B) ultrasonography scans of the pelvis demonstrated a thick-walled hypoechoic structure containing internal debris in the left lower quadrant, consistent with pyosalpinx related to recurrent tubo-ovarian abscess (arrows).
Discussion. Tubo-ovarian abscesses are often a complication of pelvic inflammatory disease in sexually active girls and women, classically resulting from sexually transmitted infections.1-6 About 18% to 34% of patients with pelvic inflammatory disease also have a tubo-ovarian abscess.2 Among nonsexually active girls and women, tubo-ovarian abscesses are rare and have been sparsely elucidated in the literature, especially in the pediatric population.3 Only 5 cases of nonsexually active girls and women aged younger than 24 years old were noted in a retrospective review of 122 cases of tubo-ovarian abscess from 2002 to 2014 in a tertiary academic center.4 Three cases of nonsexually active pyosalpinx, another complication of pelvic inflammatory disease, have been described, with a mean age of 13 years.3 The largest case series published in the literature included 16 menarchal adolescents with mean age of 14.6 years at diagnosis of tubo-ovarian abscess.2
Few mechanisms have been postulated to explain tubo-ovarian abscesses in virgin girls and women, but the exact mechanism remains unknown. Proposed mechanisms include:5
- Direct ascension of bacteria through the urogenital tract after vaginal voiding from pooling of urine in the vagina, usually secondary to obesity
- Direct spread of infection from gut translocation
- Rarely, hematogenous spread from transient bacteremia
The mechanism by which tubo-ovarian abscesses develop in virgin girls and women also depends on the patient’s comorbidities, including history of recurrent urinary tract infections, obesity, inflammatory bowel disease such as Crohn disease, and prior pelvic surgery.2,5,6
A rarer phenomenon is recurrent tubo-ovarian abscesses in a nonsexually active girl or woman, such as with our case. Recurrent tubo-ovarian abscesses have been briefly described only once in the literature.2 Our patient was obese, with an incidental finding of arcuate uterus. How this uterine anatomic variation could have predisposed our patient to tubo-ovarian abscess remains unknown.
In addition, results of a fluoroscopy were concerning for a noncommunicating left uterine horn. Follow-up pelvic MRI scans revealed that our patient did not have a noncommunicating horn. However, obesity could have played a role in the vaginal pooling of the urine, which could have caused an ascending infection. Moreover, the growth of Bacteroides thetaiotaomicron twice and Streptococcus bovis in our patient—both are gastrointestinal tract commensals—suggests that direct gut translocation could have possibly played a role in the pathogenesis of her tubo-ovarian abscess.
As tubo-ovarian abscess is a complication of pelvic inflammatory disease, it is often challenging to diagnose in sexually inactive girls and women. The diagnosis of tubo-ovarian abscess is often not straightforward and is compounded by the first-line use of transabdominal ultrasound as an empiric imaging modality, which has not been evaluated in large studies to diagnose tubo-ovarian abscess.2 As a result, it often yields nondiagnostic impressions and, therefore, may sway clinicians to an alternative diagnosis and delay therapy. Therefore, it is imperative to make a prompt diagnosis using more-sensitive imaging techniques in order to initiate management, since it is an emergent and potentially life-threatening infection. Furthermore, timely intervention is warranted in order to prevent serious complications, such as ovarian vein thrombosis, ectopic pregnancy, chronic pelvic pain, and irreversible tubal scarring that can lead to infertility.1,2
Neisseria gonorrhoeae and Chlamydia trachomatis are the usual putative infectious agents, although most cultured samples from surgical specimens surprisingly yield polymicrobial growth.1,2 It is hypothesized that both N gonorrhoeae and C trachomatis facilitate invasion of the upper genital tract by microbial flora from the lower genital tract, promoting the development of an infection.1
Data on consensus treatment for tubo-ovarian abscesses in virgin girls and women is limited. Prompt initiation of broad-spectrum antibiotics and drainage by an interventional radiologist are the usual interventions in reported cases with favorable outcomes.
To our knowledge, our case is only the second case of recurrent tubo-ovarian abscesses described in the literature. While tubo-ovarian abscesses in virgin girls and women are rare, it is crucial to recognize them in the differential diagnosis of a virgin adolescent who presents with abdominal pain, since the risk of serious acute and chronic complications is significant. It is also prudent to recognize that tubo-ovarian abscesses in virgin girls and women can be recurrent, such as in our case, which warrants high index of suspicion and prompt management.
References
1. Chernick LS. Tubo-ovarian abscesses in nonsexually active adolescents: a rare but consequential miss. J Adolesc Health. 2019;65(2):175-176. https://doi.org/10.1016/j.jadohealth.2019.04.006
2. Hakim J, Childress KJ, Hernandez AM, Bercaw-Pratt JL. Tubo-ovarian abscesses in nonsexually active adolescent females: a large case series. J Adolesc Health. 2019;65(2):303-305. https://doi.org/10.1016/j.jadohealth.2019.02.009
3. Pfeifer CM, Williams LE, Veltkamp JG, Lagomarsino EM. Pediatric pyosalpinx without sexually transmitted infection: a report of 3 cases. Radiol Case Rep. 2019;14(4):501-504. https://doi.org/10.1016/j.radcr.2019.02.001
4. Cho HW, Koo YJ, Min KJ, Hong JH, Lee JK. Pelvic inflammatory disease in virgin women with tubo-ovarian abscess: a single-center experience and literature review. J Pediatr Adolesc Gynecol. 2017;30(2):203-208. https://doi.org/10.1016/j.jpag.2015.08.001
5. Goodwin K, Fleming N, Dumont T. Tubo-ovarian abscess in virginal adolescent females: a case report and review of the literature. J Pediatr Adolesc Gynecol. 2013;26(4):e99-e102. https://doi.org/10.1016/j.jpag.2013.02.004
6. Simpson-Camp L, Richardson EJ, Alaish SM. Streptococcus viridans tubo-ovarian abscess in an adolescent virgin. Pediatr Int. 2012;54(5):706-709. https://doi.org/10.1111/j.1442-200x.2012.03569.x


