Peer Reviewed
Neck and Shoulder Pain After a Mountain-Biking Fall
Author:
Jason Le, DO
Naval Flight Surgeon for Command Training Air Wing 1 at Naval Air Station Meridian, Mississippi
Citation:
Le J. Neck and shoulder pain after a mountain-biking fall. Consultant. 2019;59(3):69-70.
Disclosure:
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, the Department of Defense, or the US Government.
A 26-year-old right-handed man and student naval aviator presented with dull, achy, nonradiating pain at the sternoclavicular (SC) joint and inferior right sternocleidomastoid (SCM). He rated the pain as 2 of 10. He denied numbness, tingling, or weakness of his right upper extremity. He reported a mild decrease in right shoulder range of motion (ROM) due to the pain. The mechanism of injury had been a fall onto his posterior right shoulder after having been flown forward from his mountain bike 2 days ago.
Physical examination showed abrasions on his posterior right shoulder, significant edema of the inferior right SCM and surrounding tissues of the right SC joint, and yellow skin discoloration on the right sternal chest wall. Musculoskeletal and neurovascular examination findings of the neck and shoulders were otherwise normal except for difficulty getting the right shoulder abduction to 180°, as well as decreased neck ROM in left rotation and right side-bending due to pain.
Radiographs of the right shoulder were taken (Figures 1-3).
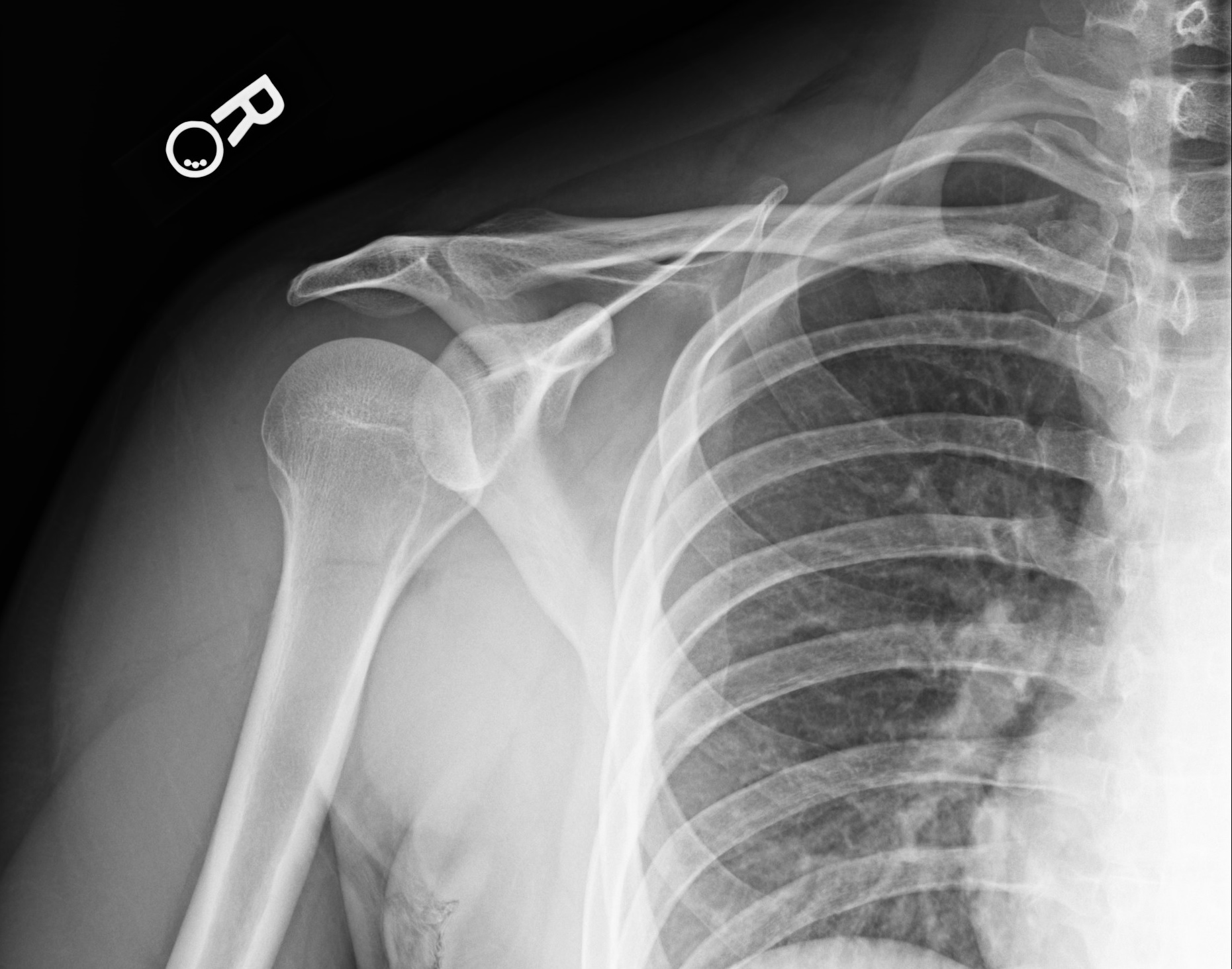
Figure 1. Anteroposterior view of right shoulder, internal rotation.

Figure 2. Anteroposterior view of right shoulder, external rotation.

Figure 3. Scapular Y view of right shoulder.
Answer: Clavicle Fracture
The patient has a clavicle fracture—more precisely, a closed, inferiorly displaced, proximal clavicle fracture.
This case was a missed read by the radiologist. I requested a re-read of the radiographs, because I was able to view the images myself. Otherwise, I would have relied on the initial read, given the minimal symptoms and deficits and the lack of neurovascular compromise. The finding of the re-read was a proximal end clavicle fracture with a 4-mm gap and inferior displacement.
Clavicle fractures are divided into midshaft, distal, and proximal, with proximal fractures accounting for 3% to 9% of all clavicle fractures.1-4 This type of fracture usually is a result of a high-energy impact, more commonly seen in major trauma or direct blows.1-4 Diagnosis often requires computed tomography (CT) due to the ribs, vertebrae, and sternum obscuring details on plain radiographs.1,2
Proximal clavicle fractures typically present similarly to midshaft fractures, with pain at the fracture site and decreased shoulder ROM and strength due to pain.2 Skin tenting and bony deformity (or bump) at the fracture site is typically seen in displaced fractures.2 Neurovascular involvement may include hoarseness, cough, and dysphagia from compression or damage of mediastinal structures, diminished sensation over the proximal chest wall due to medial supraclavicular nerve damage, and head and neck venous congestion with diminished pulses.2,4
Differential Diagnosis
SC joint dislocation is a rare occurrence (<3% of dislocations in the shoulder region) and has a similar mechanism of injury and clinical presentation to proximal clavicle fractures.5 Dislocations are commonly anterior or posterior, with posterior more concerning due to compression of mediastinal structures.5 Anterior dislocation presents with tenting of the skin with prominent clavicle at the proximal end.5 The affected upper extremity is often adducted, with elbows at 90° and held across the chest for stability.5 Radiographic evidence if often required to differentiate SC joint dislocation from fracture.
Cervical strain, commonly seen in whiplash injuries, is often bilateral and involves the trapezius.2,4 In this scenario, the SCM may present with tenderness to palpation and with neck flexion, contralateral rotation, and ipsilateral side-bending of the affected side (action of the SCM); restricted neck ROM; possible evidence of swelling of the affected portion of the muscle; and no appreciable bony deformity at the SC joint.2,4,5
SC joint strain may occur due to stress on any of the 4 ligaments or subclavius muscle stabilizing the joint.4,5 Patients may present with tenderness to palpation, swelling at the SC joint, and limited ROM of the affected extremity due to pain. No bony deformity is present at the SC joint.
Table. Differential Diagnosis | |
Condition | Distinguishing Features |
Proximal clavicle fracture | Presents as pain at the fracture site with decreased shoulder ROM and strength due to pain. Skin tenting and bony deformity at the fracture site seen in displaced fracture. Subtle fractures negative on radiographs and may require CT for diagnosis. |
SC joint dislocation | Presentation similar to proximal clavicle fracture with skin tenting and bony deformity seen in anterior dislocation. Subtle dislocations may require CT if radiographs are negative. |
Cervical strain | Presents as pain with cervical motion or tenderness to palpation of affected muscle, often involving the SCM and trapezius. No appreciable bony deformity at the SC joint of the proximal clavicle. Clinical diagnosis with imaging is used to rule out fractures. |
SC joint strain | Presents as tenderness to palpation at the SC joint, with or without swelling, and limited ROM due to pain. No bony deformity at the SC joint. Clinical diagnosis with imaging is used to rule out fractures or evidence of arthritis. |
Treatment can be either operative or nonoperative. Indications for operative management include open fractures, comminuted fractures, neurovascular symptoms, threat of eruption through the skin, and significantly displaced fractures.2,6 Nonoperative management with sling immobilization is considered in nondisplaced or minimally displaced fractures or when surgery is contraindicated.1 Immobilization varies by age. In adults, shoulder support is recommended for 6 to 8 weeks with initiation of gentle range of motion starting after 2 to 3 weeks and progression to physical therapy at 4 to 6 weeks if needed for ROM or strength concerns.7 Patients may have difficulties adhering to immobilization, which can result in refractures and nonunion. Interval radiographs are done to look for evidence of healing or refracture.
Outcome of the case. The patient was placed in an immobilization shoulder sling at the initial visit and was referred for orthopedic evaluation. A CT scan was performed, and he was recommended for nonoperative management, with shoulder immobilization and clearance to return to unrestricted activity after 6 weeks.
References:
- Bartoníček J, Frič V, Pacovský V. Displaced fractures of the medial end of the clavicle: report of five cases. J Orthop Trauma. 2010;24(4):e31-e35.
- Armstrong AD, Hubbard MC, eds. Essentials of Musculoskeletal Care. 5th ed. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2015.
- Throckmorton T, Kuhn JE. Fractures of the medial end of the clavicle. J Shoulder Elbow Surg. 2007;16(1):49-54.
- Robinson CM, Jenkins PJ, Markham PE, Beggs I. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008;90(6):685-696.
- Morell DJ, Thyagarajan DS. Sternoclavicular joint dislocation and its management: a review of the literature. World J Orthop. 2016;7(4):244-250.
- Low AK, Duckworth DG, Bokor DJ. Operative outcome of displaced medial-end clavicle fractures in adults. J Shoulder Elbow Surg. 2008;17(5):751-754.
- Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86-A(7):1359-1365.


