Authors:
Anisha Guda, BS
Student, Long School of Medicine at UT Health San Antonio
Rajani Katta, MD
Clinical Professor of Dermatology, McGovern Medical School at the University of Texas Health Science Center at Houston
Citation:
Guda A, Katta R. Allergic contact dermatitis to acrylate chemicals in artificial nails. Consultant. 2019;59(3):84-85.
A woman in her 50s presented with a rash that had been present for 10 years. The rash had begun on her toes and then had spread to involve both feet and both hands. She was retired, and her activities included gardening, playing tennis, and cleaning her home. She had been using acrylic nails but had stopped using them due to concerns for allergy. She instead began using shellac nails.
Her prior treatments had included oral corticosteroids, clobetasol ointment, oral antibiotics, urea cream, and mupirocin ointment. She had stopped all of these treatments, and at the time of presentation had been using only petroleum jelly and neomycin ointment.
On examination, red scaly patches were noted on several fingertips (Figure 1).

Figure 1.
A skin biopsy of the finger and the feet had revealed chronic spongiotic dermatitis, and she was referred for patch testing due to a concern for allergic contact dermatitis (ACD).
She underwent patch testing with an extended series of allergens, and the results indicated strong reactions to ethylene glycol dimethacrylate and hydroxyethyl methacrylate (Figure 2). She also had reactions to several fragrance additives.
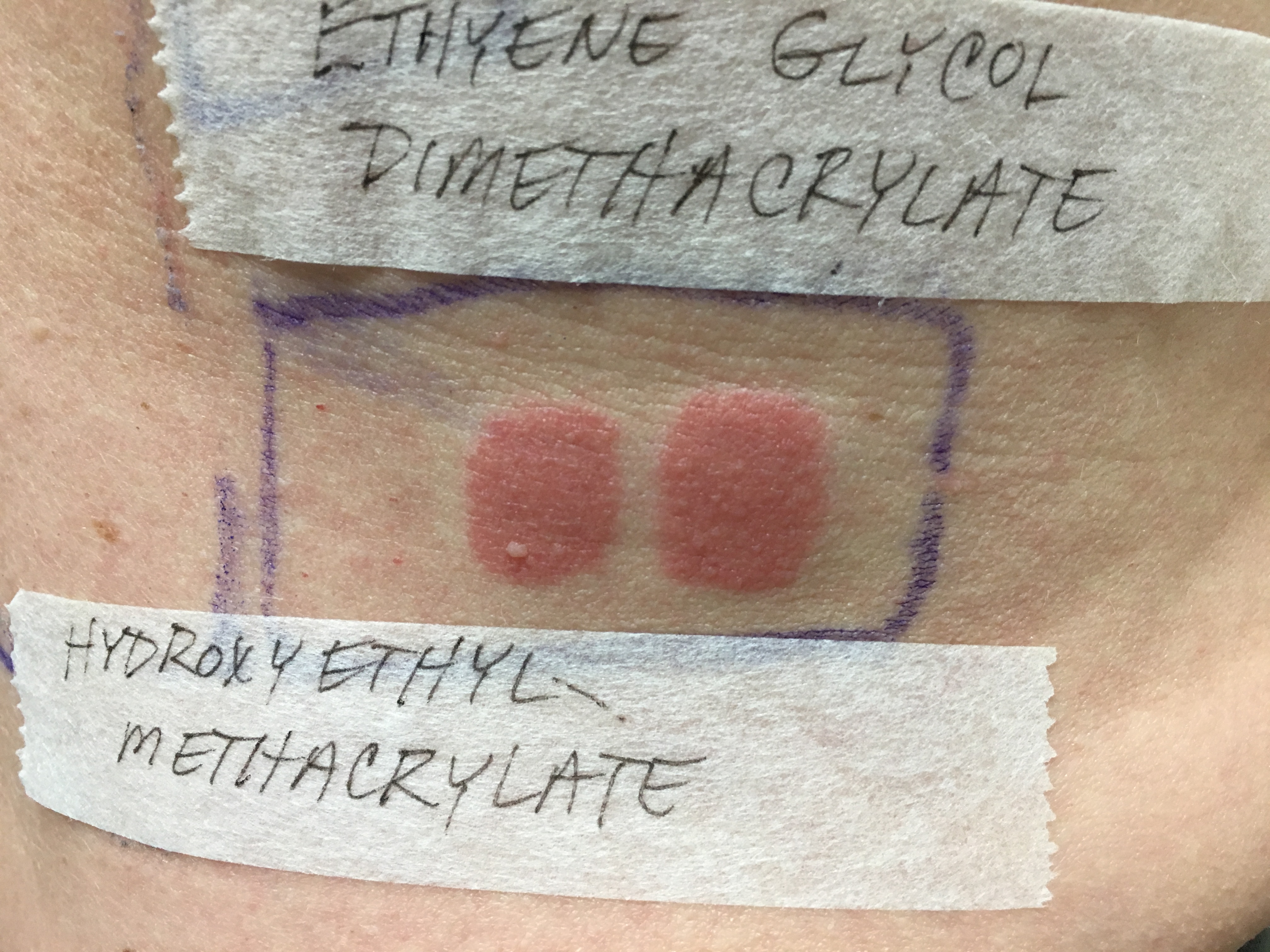
Figure 2.
To avoid the fragrance additives, she was advised about what skin care products to use. Given the acrylate allergy, she was asked to stop using all acrylic, gel, and shellac nails. She was instructed to continue clobetasol ointment to any areas of active dermatitis.
Discussion. ACD to nail cosmetics is becoming an increasing concern, especially due to misconceptions about product ingredients. ACD is also known as delayed-type hypersensitivity. Mediated by T cells, this immunologic reaction typically manifests 48 to 72 hours following skin exposure to the offending allergen. This delay in appearance of the rash means that patients may not recognize the triggering exposure and thus may need to undergo patch testing in order to identify the responsible allergens.
As in our patient’s case, nail cosmetics must be suspected as a potential trigger of hand dermatitis, as well as eyelid, facial, and neck dermatitis. The nail-service industry has grown significantly over the past decade, and studies have found an increase in consumer and occupational ACD due to nail cosmetics.1
Acrylate monomers are used in nail cosmetics and are an important allergen. Since the 1950s, the number of cases of ACD to methacrylate monomers has increased.2 Acrylates are plastic materials that are derived from the polymerization of methacrylate and acrylate monomers. The monomers are responsible for ACD; when fully polymerized, they are no longer allergenic.
Patients commonly present with an outbreak surrounding the nail plate, while more severe cases can include paronychia, onycholysis, thickened nail plates, and even nail loss. In some cases, involvement can extend to the face and neck with contact, known as ectopic dermatitis. In one review, it was estimated that up to 80% of cases may involve ectopic dermatitis of the mouth, eyelids, chin, and neck.1 Diagnosis is made through patch testing.
Management centers on effective treatment of the skin inflammation, along with extensive counseling on avoidance of allergens. Acrylates are widely used in certain settings, yet a number of popular misconceptions exist surrounding their use. One common misconception is that only acrylic nails contain acrylates. In fact, acrylates may be found in gel nails, shellac nails, dipping powder, and solar nails. While our patient suspected acrylic nails and stopped using them, she continued to receive gel and shellac nails. Shellac nails are becoming increasingly popular and may be marketed not as a type of artificial nail, but rather as a type of long-wearing nail polish. In one case series, a consumer had purchased the shellac nails over the internet.3
It is also important to recognize that acrylates also are widely used in dentistry, as bonding agents and in the creation of fillings, dentures, temporary crowns, and permanent crowns.4 They also are used in health care, including such applications as the creation of hearing aids and as bone cement in orthopedic surgery. They also may be found in other adhesives and in different industrial settings.5
As with other allergens, thorough counseling on all potential exposures is critical for successful treatment of ACD due to acrylates.
References:
- Chou M, Dhingra N, Strugar TL. Contact sensitization to allergens in nail cosmetics. Dermatitis. 2017;28(4):231-240.
- Sasseville D. Acrylates in contact dermatitis. Dermatitis. 2012;23(1):6-16.
- Le Q, Cahill J, Palmer-Le A, Nixon R. The rising trend in allergic contact dermatitis to acrylic nail products. Australas J Dermatol. 2015;56(3):221-22
- Scheman A, Jacob S, Zirwas M, et al. Contact allergy: alternatives for the 2007 North American Contact Dermatitis Group (NACDG) standard screening tray. Dis Mon. 2008;54(1-2):7-156.
- Ramos L, Cabral R, Gonçalo M. Allergic contact dermatitis caused by acrylates and methacrylates—a 7-year study. Contact Dermatitis. 2014;71(2):102-107.


